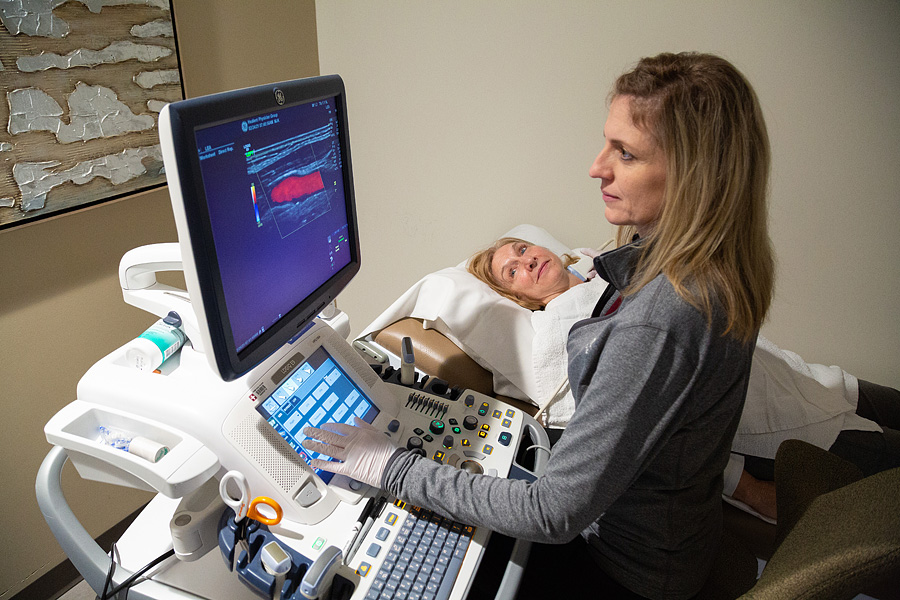
Peripheral Vascular Treatments
and Procedures
We’re proud to offer effective peripheral vascular treatments and procedures in Kansas City.
Peripheral arterial disease can be treated by lifestyle alterations, medications, angioplasty, related treatments, and surgery. A combination of treatment methods may be used.
Treatment is determined based on the size of the aneurysm, presence and severity of symptoms, and the risk of surgery. Conservative treatment is the standard for small AAA and includes an office visit with your vascular specialist and an ultrasound and/or CT angiogram every 6 – 12 months. Large or rapidly enlarging smaller AAA typically require minimally invasive surgical endograft treatment (EVAR or stent-graft placement), although open surgical repair may be needed in more difficult anatomy.
Treatment is determined based on the size of the aneurysm, presence and severity of symptoms, and the risk of surgery. Conservative treatment is the standard for small TAA and includes an office visit with your cardiac/vascular specialist and a CT angiogram every 6 – 12 months. Surgical treatment, including minimally invasive endograft repair (TEVAR or stent-graft placement) and/or open surgery, is offered when the risk of rupture is greater than the risk of the procedure/operation.
Treatment is determined based on the size of the aneurysm, presence and severity of symptoms, and the risk of surgery. Conservative treatment is the standard for small IAA and includes an office visit with your vascular specialist and an ultrasound and/or CT angiogram every 6 – 12 months. Large or rapidly enlarging smaller IAA typically require minimally invasive surgical endograft treatment (stent-graft placement) or coil embolization, although open surgical repair may be needed in more difficult anatomy.
Treatment is determined based on the size of the aneurysm, presence and severity of symptoms, and the risk of surgery. Most PAA larger than 2.0 cm in diameter require minimally invasive surgical endograft treatment (stent-graft placement), although open surgical repair may be needed in more difficult anatomy.
Treatment goals for PAD include management of symptoms and stopping the progression of atherosclerosis throughout the body. We accomplish this with medications which lower cholesterol, control blood pressure, maintain normal blood sugar levels, prevent blood clots, and dilate blood vessels. Daily walking and stopping smoking are also important for symptom improvement. For advanced cases of PAD, treatment in most cases is minimally invasive through a tiny nick in the skin to allow for atherectomy, angioplasty, stent, or stent graft placement. Advanced disease occasionally requires open surgery.
Treatment is determined based on the size of the aneurysm, presence and severity of symptoms, and the risk of surgery. Conservative treatment is the standard for small VAA and includes an office visit with your vascular specialist and an ultrasound or CT angiogram every 6 – 12 months. Surgical treatment may include coil embolization (small metal coils placed inside the aneurysm to form clot which closes the aneurysm), endograft/stent graft placement (to exclude the aneurysm from the active circulation), or open surgical repair.
Treatment includes stopping smoking, healthy diet, antiplatelet medications such as aspirin, cholesterol-lowering medications, and blood pressure control. Advanced cases of carotid artery disease may require surgical carotid endarterectomy, transcarotid stent placement (TCAR), or transfemoral carotid stent placement.
Treatment initially focuses on stopping the progression of atherosclerosis throughout the body. We accomplish this with medications which lower cholesterol, control blood pressure, maintain normal blood sugar levels, and prevent blood clots. Daily walking and stopping smoking are also important lifestyle changes. For advanced cases of subclavian artery stenosis, treatment in most cases is minimally invasive through a tiny nick in the skin to allow for angioplasty, stent, or stent graft placement.
Testing and Diagnosis for renal artery disease begins with a physical exam by a cardiovascular physician. Duplex ultrasound may help identify blockages in the kidney arteries. Computed tomography (CT) or magnetic resonance (MR) angiography are noninvasive methods of creating a “road map” of the arteries to identify the narrow areas. Catheter-based angiography involves placing a tiny tube inside the artery to give highly detailed pictures of your arterial anatomy.
Treatment for acute/sudden onset mesenteric ischemia may require immediate surgery. Chronic mesenteric ischemia is most often treated with minimally invasive surgery through a tiny nick in the skin to allow for angioplasty, stent, or stent graft placement.
Treatment of chronic venous insufficiency begins with conservative measures such as wearing compression stockings on the legs, intermittent leg elevation throughout the day, and skin lubrication. If symptoms progress to become life-style limiting despite adequate conservative measures, then minimally invasive procedures such as endovenous ablation to eliminate the ineffective superficial veins may be needed. If there are pelvic venous outflow obstructions causing the ineffective venous return from the legs, then angioplasty and stent placement in the pelvic veins may be required.
Treatment for vertebral compression fractures includes rest and over-the-counter pain medications. With severe back pain, muscle relaxants, opioid pain relievers, and back bracing may be required. If conservative therapy does not relieve the pain and allow the person to return to normal activities, a minimally invasive surgery through a tiny nick in the back’s skin called vertebroplasty or kyphoplasty may be needed. These procedures inject medical cement into the fractured vertebral body to relieve the pain.

We realize you have a choice of doctors and we value you as a patient. We believe it’s important to be caring, empathetic, and to treat each patient with dignity.
Meet your specialist.